Well, here we are, on a journey I never anticipated. Our first was an easy conception, easy pregnancy (other than a lot of all day morning sickness for the first 16 weeks), and lovely home birth. Feeding was a different story, but was also eventually successful.
So, I didn’t anticipate having fertility issues this time around. But after no positive tests for a year and half, then an early miscarriage, then a ruptured ectopic that destroyed one tube, here we are, doing IVF.
But I’ve realized through lots of questions from family, friends and colleagues, that the process of IVF is still a big mystery to most people. Whether they haven’t known anyone close to them who has gone through IVF, or whether they do know someone who has been through this process but didn’t tell anyone or didn’t go into detail — either because it worked the first time out of the gate and they didn’t dwell on it; or because they are dealing with feelings of like frustration, despair, anxiety, etc.; or whether they are fearful that sharing their infertility struggles will cause shame them — there is a ton of mystery shrouding this process. Hell, I thought I knew what I was in for, because I research EV-RY-THING, but I didn’t really get it until I completed my first cycle.
While every person has the right to decide how much to share about their journey, for me, I find it helpful to be upfront and proactive in telling people around me what’s going on. But hardly anyone understood what exactly goes into this whole process. So, I’m happy to demystify some of the logistics for those preparing for the IVF process, wanting to help a loved one through the process, or are just curious.
I’m breaking this into two parts:
- Part 1: A Layperson’s Overview of the IVF Process
- Part 2: My IVF Journey
When/Why IVF?
IVF stands for In Vitro Fertilization, a specific type of Assisted Reproductive Technology where medications and science control many (but not all) of the factors surrounding conception/early pregnancy.
There are many situations I’m aware of where IVF may be a recommended course of treatment, including:
- Fallopian tubes that have been damaged, tied, or removed — thus an alternate method is required to bypass the Fallopian tubes in order to allow sperm and egg to meet and an embryo to end up in the uterus
- Age, since our eggs have been in our bodies since we grew in the womb — the older we get, the lower our egg quantity and the lower the egg quality becomes; so it may be necessary or recommended to speed up the conception process for best results, or to select the eggs and sperm most likely to succeed at producing a pregnancy
- Low sperm quantity or quality, either motility or morphology, can contribute to poor natural fertilization rates
- Genetic issues with one or both parents that might lead a couple to decide to do IVF to be able to genetically test their embryos
- Serious medical conditions or treatments for medical conditions that may damage fertility — planning ahead to preserve family planning options following resolution of the medical condition might be a consideration
- The need to use a gestational carrier — previous medical treatments and surgeries, such as removal of the uterus, or any medical condition that would make it dangerous for someone to physically carry a pregnancy to term can mean needing to use a gestational carrier; some LGBTQIA+ parents may need to use gestational carriers, depending on the combination of their and their partner’s assigned sexes at birth, any gender confirmation surgeries that may have occurred, sometimes a need to avoid the dysphoria of carrying pregnancy, or other considerations
This is not an exhaustive list. I’m sure there are plenty of other scenarios that IVF might be recommended; please check with a fertility specialist if you have questions about your medical history, as I am providing this info for groundwork only, not as medical advice.
Also, it is possible that not all the above scenarios would absolutely require IVF either. Your medical history is unique and your comfort level and desire for various levels of intervention are also important factors that should be discussed with your doctor as you make decisions about expanding your family.
What Happens During IVF?
Again, just to give people a patient/layperson’s general idea of the process — because it’s so often shrouded in mystery for those new to it, friends and family — this is a pretty basic outline of the IVF process:
1. When You Will Begin Your IVF Cycle
At some point you will have had the discussion with your fertility specialist about IVF and have chosen to move forward, and then you will discuss what your timeframe is.
There are a couple of factors I’m aware of that can affect how soon you can start:
- Some programs have a max number of patients that they will take in a particular cycle knowing the limits of their resources (available monitoring appointments, staff, timing of procedures, etc.) and that may determine when you can get on the schedule.
- Another factor is whether your doctor/clinic does a “rolling schedule” (there might be a particular name for this — if there is I don’t know it) where they have enough resources (fertility specialist, embryologist, anesthesiologist, etc.) available all the time to take you whenever you start your cycle. (The first day of your period is considered Cycle Day 1.) In other offices, like with my doctor, they condense everyone onto a particular schedule by using birth control prior to the start to get all the IVF clients for that month into a similar cycle, because they have retrievals and transfers only during a certain window of time each month when they have the embryologists and an anesthesiologist on-site.
- A third factor could be if there are any procedures that your doctor wants to perform prior to doing an IVF cycle.
2. Filling Your Prescription
Prior to the start of your IVF cycle, your doctor will determine a medication protocol for you. This may be fine tuned over the course of your IVF cycle, but you will be given a prescription to start with so you can have your medications on-hand.
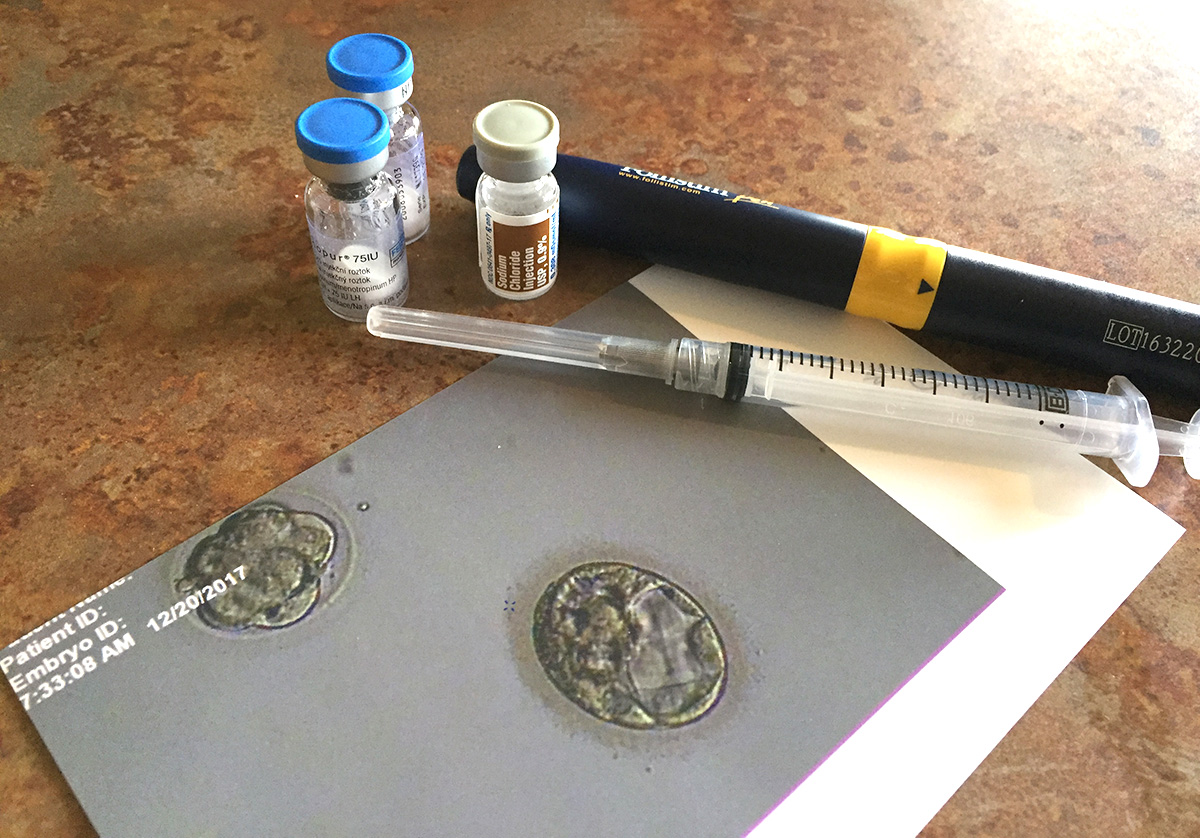
3. Starting Medications
Following your Cycle Day 1 of the cycle you will be doing IVF, your clinic will tell you which medications to begin taking, and when to start. Once you start your medications to stimulate egg development, you are then in what is commonly referred to as “stims.” Additionally, after a few days, another injection will be added, to prevent ovulation from occurring prior to retrieval. Most of the medications are given as injections, typically to the lower abdomen. I have now completed three full IVF cycles, and at various points I have been on 1, 2, 3 or 4 injections a day. These medications should be taken at the same time each day, so picking times that you can be consistent with is important.
4. Ultrasound Monitoring & Bloodwork
You will also start having your monitoring ultrasounds. These are internal ultrasound scans performed periodically during follicle development so the doctor can monitor the growth and development of the follicles, count the number of growing follicles, determine whether to adjust the dosage of your medications, and start to extrapolate your retrieval date. They are also tracking the growth of the uterine lining to make sure it is thickening enough to allow a pregnancy to implant.
Bloodwork taken at the monitoring appointment is common, to track hormone levels and other factors that could affect outcomes.
5. Scheduling Egg Retrieval/Taking a Trigger Shot
When it is determined that your eggs appear to be reaching maturity, your egg retrieval day and time are scheduled and you are instructed to take a trigger shot. The trigger shot triggers ovulation and its timing is very specific so that it is a certain number of hours before your egg retrieval will happen.
You will likely also be put on a short round of antibiotics, to prevent any infections from the retrieval, and would start the antibiotics prior to the actual retrieval.
6. Egg Retrieval
Egg retrieval is a surgical procedure, done under anesthesia so that you are asleep. So, you will have to prepare for this like any other general anesthesia event: no food or drink a certain number of hours prior to the procedure. You will go in and change into a hospital gown, and get an IV.
When it is your turn for retrieval, you will go into the procedure room and be given the anesthesia. When you are under, a scope and needle are inserted into the vagina, through the cervix, into the uterus, then pierce the uterine wall, and up to the ovaries. The eggs are then removed by needle aspiration and collected.
While eggs are being retrieved, if fresh sperm are being used, your spouse/partner will be asked to provide that. If using frozen sperm or frozen donor sperm, the lab likely already has that.
If you are planning to do a fresh transfer, this is also the day that you will begin your intra-muscular shots of Progesterone, to help support and sustain the intended pregnancy.
7. Fertilization
The collected eggs are given to the embryologist for fertilization. The method can vary, from putting sperm and eggs together and letting them self-fertilize (conventional IVF method), to selecting specific individual sperm and injecting them into each egg (called ICSI, or Intracytoplasmic Sperm Injection), or a combination of both. (Some facilities may do up to a certain number of eggs as ICSI and the rest conventional.)
8. Waiting, and Watching The Embryos Grow
Then the embryologist(s) “babysit” the embryos to see what happens. Hopefully you get high quality embryos that are dividing and growing well, and possibly have extra to freeze.
9. Final Decision on Where the Embryos Are Going
What happens next depends on a few factors, either freezing all embryos that look good, or doing a fresh transfer of embryos.
- Freezing/Storing — Freezing embryos may happen for a couple of different reasons. For some couples, going through the IVF process and freezing embryos is a proactive move because they don’t want a family yet, but want to take advantage of better fertility while they are younger, preparing for some major medical treatments that could affect fertility, or are otherwise preparing for a family at a later date — either weeks, months or years later. For others, they are freezing because they have decided to do genetic testing of their embryos, and that process takes a few weeks to get results, so the embryos are frozen in the meantime.
- Fresh Transfer — Fresh transfers happen several days after retrieval. At the clinic I use, it is either 3 days or 5 days after fertilization. 5 day is their optimal, as the embryos will have divided and grown enough to become a blastocyst or close to it. A blastocyst is when the cells have continued dividing and which has begun to differentiate into inner cells and outer cells. Earlier transfers may happen if embryos are looking fragile and putting them into the most ideal environment, your uterus, would give them the best possible chance.
If you have more embryos than would be responsible/ethical to transfer at once, you may have both a fresh transfer and have some to freeze.
How many are embryos are transferred is a discussion between you and your doctor. Depending on how many you have, you and your doctor ethically need to find a balance between increasing the likelihood of pregnancy, but reducing risk of multiples.
10. Transfer
On the day of transfer, you will have to drink a bunch of water and then not use the bathroom. The reason is because a bladder full of urine shows up as a large dark area on the ultrasound. This helps the doctor to see the uterus more clearly defined so that it’s easier to visualize the uterus, and the catheter going into the uterus.
You will likely be put in a hospital gown, and then go back into the procedure room, only you are awake for this part.
An abdominal ultrasound will show if you have enough urine and if your endometrial (uterine) lining is the proper thickness to allow implantation. If everything looks good, they will proceed. First they insert the speculum. Then they use a saline wash to clean the vagina and cervix to reduce the possibility of infection.
Then the catheter will be inserted into the vagina, through the cervix, and into the uterus to a location and depth that the doctor determines. And then they release the embryos. They look like little white sparkles that suddenly appear on screen. (It’s not actually the embryos you are seeing, as they are too tiny at that point, but rather the fluid that surrounds the embryos.) This is a bizarre moment, trying to focus on the miracle going back into your body — while also trying not to pee on your doctor.
11. Two Week Wait
It’s not always exactly two weeks of waiting, sometimes more like 11-12 days, but it is commonly referred to as “the Two Week Wait.” This is the period of time in which the embryo(s) will hopefully continue to grow, divide, implant, and begin a healthy, in-utero pregnancy. The body will not begin to produce detectable levels of Human Chorionic Gonadotropin (hCG) until right before you are due for a period.
This is a very strange time, as there is very little left for you to do, except for observing a pelvic rest protocol, to continue taking your vitamins and supplements, perhaps taking it a bit easier than you normally would, after having such an intense lead-up prior.
You may be tempted to try taking a home pregnancy test. The tricky part is that if you try testing too soon, you may get a positive, but it may be the hCG from your trigger shot, not from a pregnancy.
12. Testing
At the end of the Two Week Wait, you will have orders for a blood draw. And then you wait for the news from the office, hoping for good news.
If the first blood draw is positive, you will have a second test two days later to confirm hCG is increasing as anticipated for a healthy pregnancy. (hCG doubling every 48-72 is considered the desirable rate of hCG for healthy pregnancies.)
13. Ultrasounds
If the pregnancy continues as anticipated, something should be visible by internal ultrasound when hCG reaches 4,000-6,000.
A later ultrasound should confirm a heartbeat. After that point, it is up to your specialist when to refer you back to your OB or other pregnancy care provider(s).
So, that’s the whole process in a nutshell, for the uninitiated. If you’re interested in more of a personal account about the whole process, Part 2: My IVF Journey is coming soon.
Special thanks to each member of my wonderful fertility team, Dr. Simckes, Ashley, Denise, and the rest of the staff at Fertility Partnership, who have held me in such love and support during my entire fertility and IVF process.

 Email
Email